Introduction
There are many types of surgery for the treatment of glaucoma that your ophthalmologist may discuss with you, e.g.:
• Trabeculectomy
• Trabeculotomy
• Tube surgery (also known as tube shunt, glaucoma drainage device, aqueous shunt)
• Cataract surgery/Lens extraction
• Deep Sclerotomy
• Goniotomy
• Iridectomy
• Viscocanalostomy
• Minimally Invasive Glaucoma Surgery (MIGS) devices
There are many unique factors about you as a patient, as well as the condition of your eye, and the level of progression of your glaucoma, which will determine which surgery is the most appropriate to treat your condition at any particular time. Laser procedures are also available and are discussed on another section of this website.
Below are descriptions of some of the most common surgeries that you are likely to have to treat your glaucoma.
Trabeculectomy
Trabeculectomy is the most common type of glaucoma surgery performed worldwide
It is done under local anaesthesia in most cases as a day case.
It involves creating a flap in the sclera (the white part) of the eye just under the upper eyelid. This flap is then loosely tied down with sutures such that some fluid can leave the eye and flow under the conjunctiva (the transparent ‘skin’ of the eyeball). In this way the eyeball pressure can be lowered, resulting in a ‘bleb’ or raised area of conjunctiva which can be visible under the upper eyelid.
Trabeculectomy surgery takes around half an hour and can sometimes be performed at the same time as cataract surgery.
Why do I need surgery?
Glaucoma is an eye disease that is often associated with elevated eye (intraocular) pressure, in which damage to the optic nerve can lead to loss of vision and even blindness. In order to lower the eye pressure, eye drops and sometimes laser can be used. But when those measures are inadequate to lower the eye pressure, it may be necessary to do an operation, called trabeculectomy.
Aims of surgery:
To lower eye pressure by channelling fluid from the eye to drain externally
To reduce dependence on pressure- lowering eye medication

Clinical image of a bleb

The flow through a “bleb”
Tube Surgery
This type of glaucoma surgery is usually reserved for more severe cases, typically if a patient has had trabeculectomy which longer longer works properly.
In Singapore the 2 most common types used are the Ahmed implant and the Baerveldt implant. Both are similar and your surgeon will choose the most appropriate device for you.
The implants consist of a drainage plate which is usually (but not always) sutured to the top of the eyeball underneath the upper lid. Attached to the plate is the plastic tube which is inserted into the anterior segment of the eyeball allowing for the fluid within the eye (known as the ‘aqueous) to drain via the tube, into the plate and subsequently out of the eye.
The idea, just like in most glaucoma procedures, is to lower the eye pressure. The surgery usually takes a little longer, approximately one hour, and the risks and complications are different to those that can occur in trabeculectomy.
Why do I need tube surgery?
Glaucoma is a disease of the optic nerve and usually the eye pressure is too high for your own eye. If uncontrolled, blindness can result from damage of the optic nerve. In order to lower the eye pressure, eye drops and sometimes laser can be used. But when those measures are inadequate to lower the eye pressure, sometimes it is necessary to do an operation.
A glaucoma drainage device implantation is usually only performed after medications, laser procedures and other surgical procedures (e.g. trabeculectomy) have failed or are deemed unsuitable. In certain types of glaucoma, a glaucoma drainage device may be considered as the first surgical procedure due to high risk of failure of other procedures.
What is a glaucoma drainage device?
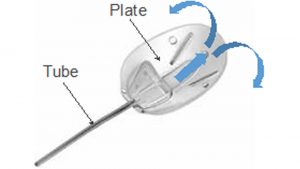
A glaucoma drainage device is a small device that is implanted to reduce the eye pressure. There are two main parts to the device, a tube and a plate.
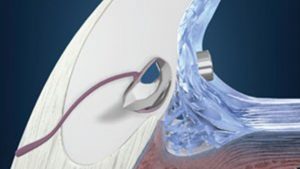
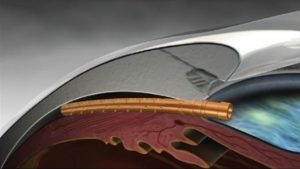
The tube is made up of silicone and is inserted into the front chamber of the eye through a small hole to drain fluid from inside the eye to the plate that acts like a reservoir for this fluid. The plate is attached to the white wall (sclera) of the eye and is covered by the conjunctiva (covering of the eyeball) so it is not visible. The drained fluid is then absorbed back into the blood through blood vessels in the conjunctiva.
The most commonly used device in SNEC is the Ahmed valve implant. This surgery is done as a day procedure so you can go home on the same day. The surgery takes about 30 to 45 minutes. Before the surgery, the surgeon will give a local anaesthetic injection around the eye to numb the area and light sedation will also be given by the anaesthetist.
It is important to know that this operation is not done to improve your vision. It is performed to help lower the eye pressure, and preserve your vision in the long term.
- The Ahmed Glaucoma Valve Implant
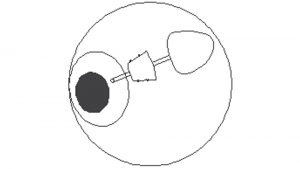
- Placement of the tube device
What are the risks and complications of a tube surgery?
Infection
As with any surgery, tube surgery will carry the risk of infection. Infections are rare and most can be treated with topical antibiotics (eye drops). The more serious infections are even rarer, but they can lead to permanent loss of sight. It is important to inform the ophthalmologist if you experience the onset of eye redness and pain after surgery.
Bleeding
This can occur at the front or back of the eye, or at the outer covering of the eye. Bleeding at the front of the eye and outside the eye is usually mild and short-lived. Bleeding at the back of the eye can lead to loss of sight but this is rare. You must inform the surgeon before operation if you are taking any blood-thinning medications.
Eye pressure is too low
Although steps are taken to reduce this risk, it may still happen and can lead to reduced vision. The good news is that vast majority of such cases will settle by itself and the vision will return to normal. However, if the eye pressure is too low for a long period of time, or if it is so low that it causes other problems, the surgeon may need to inject a “jelly-like” substance into the front of the eye in the clinic or take you back to the operating theatre to adjust the implant. Usually this is successful and the eye pressure will return to an appropriate level.
Eye pressure is too high
In the early period after surgery, the tube may be blocked by proteins or blood but this usually settles when they dissolve. The eye pressure can sometimes be high six to eight weeks after surgery as some scarring may occur around the plate. This is a normal response to implanted devices in the eye. Your ophthalmologist may restart the pressure-lowering eye drops to reduce the eye pressure.
Wound leak
This can happen if there is poor wound healing. Some cases can settle with non-surgical intervention. However, the surgeon may need to take you back to the operating theatre for wound resuturing if the wound leak does not resolve or if it causes other problems.
Damage to the lens or cornea
During tube surgery, the small protruding tube portion of the implant will be placed at the front of the eye and it may cause damage to structures of the eye, such as the lens or cornea. Your surgeon will take extra care to position it carefully but if it causes constant touch to the lens, cornea or other structures, you may need to be taken back to the operating theatre to reposition it.
In extreme cases of tube-corneal touch, the cornea may lose its clarity and a corneal transplant may be necessary.
Cataract formation
A tube surgery can also result in worsening of your cataract which is why some surgeons may recommend performing a combined cataract and tube surgery at the same time. If your surgeon decides not to perform the combined surgery, you can develop cataract later. When it causes significant reduced vision, a day surgery can then be performed to remove the cataract.
Tube / plate-related complications
- Exposure
The plate is secured onto the white wall (sclera) of the eye and the tube is covered with a sclera patch and the outer covering (conjunctiva) of the eye. However, the covering may thin out with time and cause plate or tube exposure. Further surgery will then be necessary to patch it up to prevent infection. In some cases, removal of the implant may be necessary but this is very rare.
- Movement / migration of the implant
Rarely, the stitches holding the plate may break or loosen with time, causing the implant to move. This can cause movement of the tube, resulting tube touch to structures within the eye, or eye retraction with tube failure. Tube repositioning in the operating theatre may then be necessary.
- Double vision
This is uncommon after a tube surgery, especially with the Ahmed valve implant. The surgery or scarring and fibrosis may interfere with the muscles of the eye and cause double vision. This is usually temporary but some cases may need further surgery to alleviate this complication.
– Sudden loss of vision (wipe-out)
In patients with late-stage glaucoma, there is very little healthy optic nerve left, so any surgery to the eye can result in the loss of the remainder of the optic nerve. However, this complication is very rare.
It is important to note that although surgery poses risks, not having surgery also carries the risk of progressive blindness if the eye pressure is not well controlled.
What should I expect after the surgery?
You will be reviewed the next day after surgery. Frequent follow-ups will be required in the first few weeks after surgery. The timing of follow-ups and future reviews depends on your recovery.
Most of the time, the vision in the operated eye may be reduced in the first few weeks or longer. It may take about two to three months for the vision to stabilise, sometimes even longer in complicated cases.
The eye may feel a bit sore or prickly due to the stitches in the eye. This should get better a few days to weeks after surgery. If your eye is recovering well but worsens suddenly (i.e. more pain and redness or worse vision), you should inform your ophthalmologist immediately.
You will receive a prescription for eye drops after surgery, typically steroid (for treating inflammation) and antibiotic (for preventing infection) eye drops. It is important that you instill the eye drops as instructed. After the surgery, you will no longer need to use your previous glaucoma eye drops. However, in the longer run some patients may need to restart these to lower the eye pressure to an appropriate level. In your other eye, you should continue with any glaucoma eye drops as before.
Is my glaucoma cured? Will I need further surgery?
There is no cure for glaucoma. Surgery is done to lower the eye pressure to reduce the risk of further visual loss. In general, surgery provides an alternative route for the fluid inside the eye to drain out, thereby lowering the eye pressure to a safe level.
Tube surgery can and often does keep the eye pressure low for several years. Some operations may start to work less well after a period of time. This depends on many factors such as age of the patient, type and severity of the glaucoma, etc.
If the surgery fails to keep the eye pressure to an appropriate level, your ophthalmologist may prescribe pressure-lowering eye drops to you. In some cases, patients may need to have further glaucoma surgery if the eye pressure becomes inadequately controlled.
Please consult your surgeon if you have any further queries about the surgery.
MIGS
Minimally Invasive Glaucoma Surgery
What is “Minimally Invasive Glaucoma Surgery”?
Minimally Invasive Glaucoma Surgery, also known as “MIGS” is an exciting new development in the treatment of glaucoma.
For the past few decades, the two main types of glaucoma surgery were Trabeculectomy and Tube Shunt Implants. However, these surgeries are associated with potentially serious and sight-threatening complications, hence are usually performed on patients with advanced glaucoma on whom medical treatment has failed.
In recent years, with the emergence of MIGS, the glaucoma treatment paradigm has been transformed. MIGS includes a diverse group of alternative glaucoma surgeries that are intended to be safer and less invasive compared with traditional glaucoma surgeries. They are characterized by the following features: high safety profile, less trauma, ease of use and rapid recovery.
All the MIGS procedures treat glaucoma by lowering the eye pressure.
Which glaucoma patients are suitable for MIGS?
With the higher safety profile of MIGS, these surgeries can be offered to glaucoma patients who have less severe glaucoma compared to traditional glaucoma surgery which is more appropriate for patients with advanced glaucoma.
Currently, these devices are licensed for the treatment of primary open angle glaucoma. They may be an option for patients who are unable to tolerate their glaucoma eyedrops, frequently forget to use their eyedrops or suffer from significant side effects associated with the eyedrops.
Please consult your eye surgeon regarding your suitability for MIGS.
What are the different types of MIGS devices?
There are numerous MIGS devices available. In general, these devices drain to different regions in the eye.
- Schlemm’s canal MIGS devices
- Suprachoroidal MIGS devices
- Subconjunctival MIGS devices
Schlemm’s Canal MIGS Devices
- iStent Trabecular Microbypass Stent
- iStent Inject
- Hydrus Microstent
Suprachoroidal MIGS Devices
- Cypass Microstent
- iStent Supra
Subconjunctival MIGS devices
- XEN Gel Implant
- Preserflo Microshunt
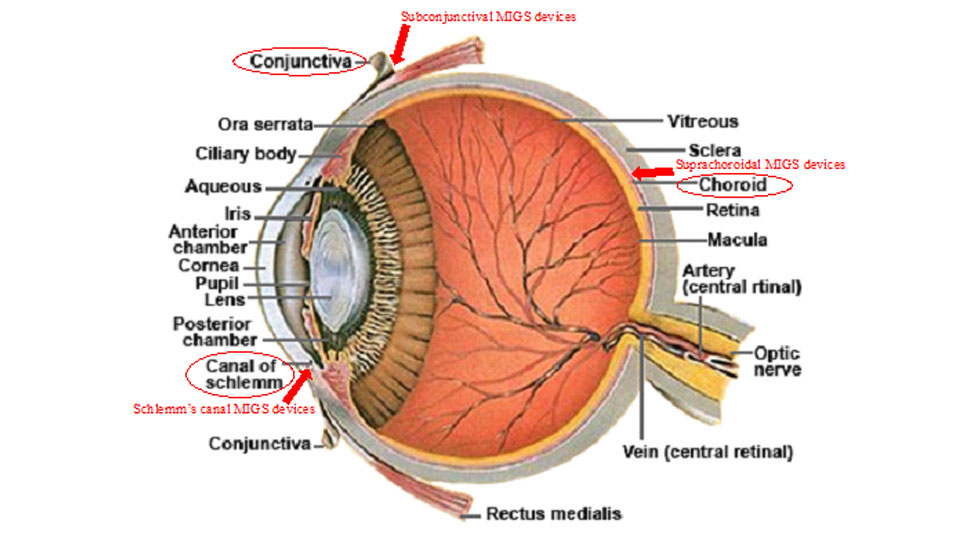
Cross-section of the eyeball, with the arrows indicating the location of MIGS devices
The various MIGS devices differ in size, material, safety profile and efficacy. Please consult your eye surgeon regarding the MIGS device which is most suitable for you.
Do all eye surgeons perform MIGS?
Specialized training is required before an eye surgeon is accredited to perform MIGS procedures. Please verify with your surgeon regarding the MIGS procedures that he/she is trained to perform.
Goniosynechiolysis
Goniosynechialysis is a procedure which is performed at the same time as cataract surgery for patients with angle closure glaucoma. This procedure is only indicated if you have significant amounts of scar tissue (known as peripheral anterior synechiae or PAS) in the drainage angle of the eye (the part where the iris meets the cornea).
It involves gentle peeling away of iris tissue from the drainage angle using a thin metal spatula. You can think of it like breaking abnormal scar tissue. If successful it allows for the drainage angle to work more efficiently and thereby lower the eye pressure.
It’s very safe and it can, in many cases, result in more eye pressure lowering to just performing cataract surgery alone.
The procedure takes about 5 to 10 minutes longer than cataract surgery alone. It is not painful.
If you are eligible for goniosynechialysis when you have your cataract surgery, the surgeon will inform you and counsel you accordingly.
Glaucoma surgery post operative care and advice
The aim of most glaucoma surgeries is to lower the eye pressure and frequently, the surgeon has to make incisions on the eye. It is important to prevent infection and large sudden reduction in eye pressure.
There are several precautions that are worth taking note.
1. Avoid unnecessary external pressure over the operated eye.
Please avoid the following:
– Squeezing or forcefully close your eyelids when instilling eyedrops. It would be easier to lean backwards or lie flat to instill the eyedrops. Alternatively, a caregiver can help to instill the eyedrops
-Not using the eye shield or placing the eye shield incorrectly (the eye shield could be pressing on the eye instead)
-Carrying heavy loads
-Rubbing your eyes with your hands
2. Use the correct eyedrops based on the instructions. There are usually 2 different types of eyedrops which typically are anti-inflammatory and anti-bacterial medications. If you need to use more than 1 eye drop each time, please allow at least 3-5 minutes interval between each eye drop. If you run out of medications before your next follow-up appointment, please contact your doctor or the outpatient clinics. If you have pre-existing glaucoma eye drops, please clarify with your glaucoma doctor if you should continue or stop them after surgery.
3. If there is significant worsening of your vision, increased eye swelling, eye redness or pain, please seek early consultation with your eye doctor. This is especially important in the early period after surgery.
4. Use your eye shield as prescribed to avoid any accidental or unintentional pressure/injury to the eye. The eye shield can be washed with clean water or alcohol sanitizer but you should dry it before applying it to the face.