Where can I get help?
If you have been diagnosed with glaucoma then you will most likely already be under the care of an eye doctor (ophthalmologist) who is also a glaucoma specialist.
They will be the best people to ask advice from as they will know your specific situation, and the best treatment for your particular situation.
Am I going to go blind?
Glaucoma is a serious disease that can result in blindness.
Thankfully most people with glaucoma will not go blind. Overall, only about 10% or less of people with glaucoma will go blind.
You are more likely to go blind from glaucoma if:
• you are diagnosed late and the glaucoma is already at an advanced stage
• you do not take your eye drops properly
• you fail to turn up for your appointments to monitor if the disease is progressing and treatment needs to be changed.
Age is also a factor in that developing glaucoma at an earlier age is more likely to result in visual loss, simply because glaucoma is a progressive disease, and a young person with glaucoma will have it for many more years than someone who develops glaucoma later in life.
Do I need to change my lifestyle?
In the vast majority of cases the answer to this question is no.
There are a few occupations/hobbies that might worsen your glaucoma such as wearing a tight necktie, playing a wind instrument, scuba diving and some yoga positions (involving inverted or upside down positions on a regular basis).
It should be noted that even for these pastimes the evidence for them causing worsening of glaucoma is fairly weak. The best thing to do if you are not sure is to check with your ophthalmologist, who will be able to advise you based on your specific condition.
If you have had glaucoma surgery, such as trabeculectomy, then usually swimming is discouraged, certainly in the first few months after surgery, as it may result in infection.
Am I allowed to drive?
The legal status regarding fitness to drive specific to glaucoma sufferers is dependent on your visual acuity in each eye, and your visual field (with both eyes open).
It is also dependant on what class of vehicle you intend to drive, for example if you will be driving a bus or taxi.
Please inform your doctor if you have are not sure regarding your legal status to drive and they will advise you what eye test you need to take. If you notice that you have any problems with your vision and are concerned about driving, then please stop driving and arrange to see an ophthalmologist as soon as possible.
How is glaucoma treated?
The aim of glaucoma treatment is to prolong visual function for as long as possible with the minimum of side effects and discomfort. In practical terms this means lowering and/or controlling the eye pressure, or intraocular pressure (IOP), because many studies have shown that by lowering IOP it is possible to slow down or even halt the deterioration in visual function caused by glaucoma. Sadly, damage to the optic nerve is permanent and it is not possible to reverse the changes that have already occurred.
There are 3 main ways to lower the IOP; eyedrops, lasers and surgery. The method of treatment will be decided by your eye doctor.
Modalities of Treatment
Laser treatment
For angle-closure type of glaucoma
- Patient undergoing laser treatment for glaucoma
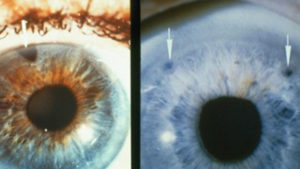
- Laser treatment (white arrows) for angle closure glaucoma
Medications
- Different type of eyedrops for glaucoma – all are meant to reduce the eye pressure
Surgery
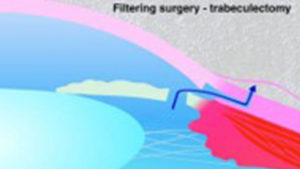
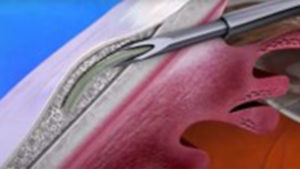
-Trabeculectomy
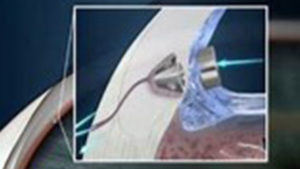
-Tube Implant Surgery
-Minimally Invasive Glaucoma Surgery
- Trabeculectomy
- Tube Surgery
- Minimally Invasive glaucoma surgery
- Minimally Invasive glaucoma surgery
Whatever the modality of treatment,
The aim is for reduction in Intraocular Pressure (IOP), with the aim of keeping IOP at a level low enough that will preserve remaining nerve function and prevent further damage
Key to this is:
• Regular follow up appointments to monitor the progression of the glaucoma and the IOP
• Compliance with medication and taking eyedrops if they are prescribed

Regular Follow up

Compliance with medication
Social Support
Medications
Some patients require help with drop instillation
This can also help decreased wastage of eyedrops
Others just need the help of a relative to remember to put drops