Humphrey Visual Field (HVF)
Patients with glaucoma experience progressive loss of their visual fields if untreated. Visual fields are often best monitored with the Humphrey Visual Field (HVF) Test. These tests are important in diagnosing glaucoma and monitoring progression.
Humphrey Visual Field is a non-invasive test that is carried out by a technician and is done in a dark room. For the test, the patient will need to place their chin on a chin rest and look at a steady, central, white light located within the machine. It is important for the patient to constantly focus on the white light to ensure accuracy of the test.
During the test, small light-spots of different size and intensity will appear at different locations in the machine. The patient will be required to press on a response button whenever they detect these light-spots. Sometimes the light-spots can be very dim and may be barely perceptible- this helps to determine how sensitive the patient is to a light stimulus at that particular point. The whole test takes about 5-10 minutes per eye. It is important that the patient is positioned comfortably prior to commencement of the test. At any point if the patient is tired, the test can be paused for breaks- this can be done by holding down the response button.
After the test is complete, it will be sent to the ophthalmologist for interpretation.
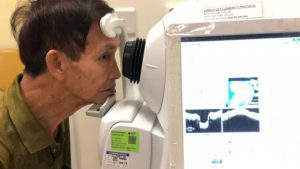
Optical Coherence Tomography Test (OCT)
Optical Coherence Tomography – Retinal Nerve Fiber Layer Test (OCT- RNFL) is an essential, non-invasive test that is used alongside visual field tests for the diagnosis and monitoring of glaucoma. The test aims to measure the retinal nerve fiber layer around the optic disc, where thinning of this layer may signify glaucoma progression. Thinning of the RNFL is also one of the earliest signs in glaucoma detection and may precede visual field changes.
The test is performed by a trained technician and takes about 5 minutes. The patient is required to place their forehead on the head-rest and chin on a chin-rest, and focus on the indicated light in the machine. Movement of patients’ eyes during the test and presence of media opacities (e.g. cataracts, cornea scar) can affect the quality of the scan.
OCT RNFL is usually interpreted together with visual field tests and clinical examination of the optic disc.
Others
Anterior Segment Optical Coherence Tomography (ASOCT)
Anterior segment optical coherence tomography (ASOCT) is a useful adjunct in the diagnosis of glaucoma. It is usually interpreted together with clinical gonioscopy to determine if the patients’ angles are open or closed. It is a non-contact test that provides high resolution images of the anterior segment, showing cross-sections of the cornea, sclera, angle structures, iris configuration and lens profile.
The test is carried out by a technician in a dim room and takes about 5 minutes. In order to obtain good images, the patient is required to hold their head still with their forehead on the head rest- and chin on the chin- rest provided.
Central Corneal Thickness (CCT)
Central Corneal Thickness or CCT for short is one of the pieces of information that your ophthalmologist will require to accurately measure your intraocular pressure (IOP). Your ophthalmologist may send you for a test to measure each eye’s CCT where numbing drops will be instilled into your eye before a machine gently touches the front of your eye to measure corneal thickness. This procedure takes less than 5 minutes and is painless.
Studies have shown that a lower CCT is a risk factor for the development of glaucoma. Patients with thin corneas can show artificially lower IOP readings than patients with thicker corneas.
Most patients who are on follow up for glaucoma or related conditions will require a CCT measurement at some point in time.

IOP Phasing
Just like blood pressure, everyone’s IOP fluctuates throughout the day. The difference may be as much as 6mmHg – and typically it is higher in the early morning. IOP phasing is a process that measures your IOP over different times of the day, usually 2 hours apart.
A numbing drop will be instilled into your eye, and your IOP will be measured with a small device that gently touches the surface of your eye. This takes less than 5 minutes.
This will be repeated at different times in the day, for examply – 9am, 11am, 1pm and then 3pm. You are free to rest in the clinic or have a meal in between.
After the final IOP measurement, your ophthalmologist may perform additional examinations and tests on your eye which may involve dilating your eyes. This may make your vision blurry. He or she will then discuss the results and your condition with you.